What Is Self-Directed Care? Definition, Benefits & 2025 Statistics
Learn what self-directed care is, how budget and employer authority work under Medicaid, and why over 1.5 million Americans use participant-directed services.
For decades, the American approach to long-term care was simple: professionals knew best. If you needed help, an agency sent a stranger to your home at a time convenient for them.
Self-direction (also known as participant-directed care) upends this model. It operates on a radical premise: the person receiving care is the best judge of their own needs.
Today, this is not just a philosophy—it is a massive engine of the Medicaid system. With over 1.5 million participants managing their own budgets and staff, self-direction has evolved from a niche pilot program into the primary solution for the nation's caregiving crisis.1
Key Takeaways
- Twin Powers: Self-direction grants you Employer Authority (hiring staff) and Budget Authority (managing funds).2
- Rapid Growth: Enrollment has surged 23% in recent years, reaching 1.52 million Americans.1
- Better Health: Participants report fewer unmet care needs and higher satisfaction compared to agency-managed care.3
- Family Caregivers: The model allows you to hire family members, solving the shortage of direct support professionals in rural areas.4
- Cost-Effective: While upfront costs can look higher due to fuller utilization, self-direction significantly lowers the risk of expensive institutionalization.3
The Twin Pillars of Authority
At its core, self-direction is defined by two distinct legal authorities granted by federal 1915(c), 1915(j), and 1915(k) waivers.3
1. Employer Authority
You are the boss. You recruit, interview, hire, train, schedule, and dismiss your workers.
- Legacy Model: An agency sends whoever is available.
- Self-Directed Model: You hire your neighbor, your cousin, or a specialist who understands your specific condition.2
2. Budget Authority
You control the money. You decide how your Medicaid allocation is spent across different categories.
- Legacy Model: Funds are locked into specific service codes.
- Self-Directed Model: You can shift funds from "respite" to "community integration" or purchase adaptive technology (like an iPad for communication) if it meets your goals.2
The Data: A Movement in Numbers
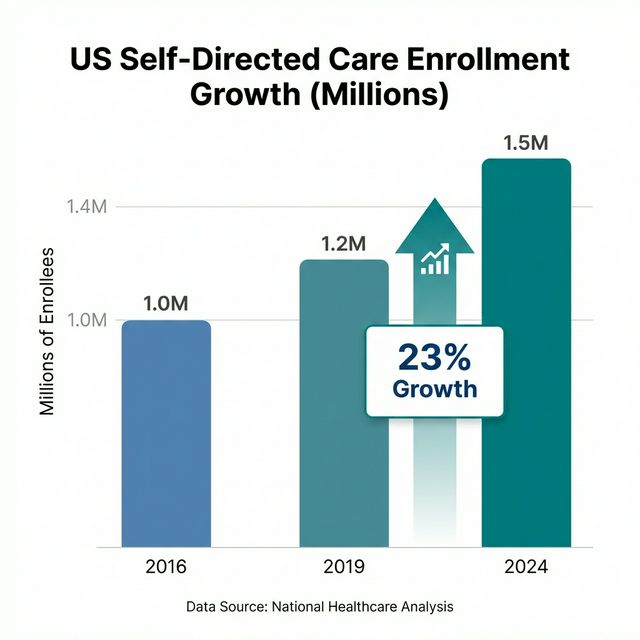
Self-direction is no longer a fringe experiment. According to the latest National Inventory of Self-Directed Long-Term Services and Supports:1
- Total Enrollment: 1,520,267 participants.
- Growth Rate: +23% since 2019.
- Funding: Medicaid pays for roughly 66% of all self-directed services in the US.
Growth Trajectory
| Year | Total Enrollment | Growth (from prior period) |
|---|---|---|
| 2016 | 1,058,889 | N/A |
| 2019 | 1,234,214 | +17% |
| 2023/24 | 1,520,267 | +23% |
This surge is driven largely by the COVID-19 pandemic, which exposed the fragility of congregate care settings (nursing homes) and accelerated the demand for home-based alternatives.5
Why It Works: Clinical & Economic Outcomes
Critics often worry about fraud or safety. "Can vulnerable people really manage their own care?"
The data says yes. In fact, they do it better than agencies.
1. Fewer Unmet Needs The Medicaid and CHIP Payment and Access Commission (MACPAC) found that self-directed participants are more likely to get the hours of care they are authorized for. Agencies often "call out" or fail to staff shifts due to worker shortages; self-directed families find a way to cover the shift.3
2. Higher Quality of Life National Core Indicators (NCI) data shows that people who self-direct are more likely to make choices about their daily routine, have friends who are not staff, and participate in their community.6
3. Solving the Workforce Crisis The US faces a shortage of nearly 8 million direct care workers by 2030.4 By allowing participants to hire friends and family (who would otherwise provide unpaid care), self-direction unlocks a massive, previously untapped labor pool.
The "Cost" Paradox
A common finding is that self-directed care helps participants spend more of their budget than agency participants.
Is this bad? No.
- Agency Reality: If an agency can't find a worker for 20 hours of your plan, that money isn't spent, but you go without a bath or a meal.
- Self-Directed Reality: You use your full budget to hire a neighbor. The "cost" to the state is higher, but you stay healthy and avoid a $100,000 hospital stay for a bedsore or UTI.3
Frequently Asked Questions (FAQ)
1. Who helps me manage the paperwork?
You are never alone. You are required to use a Fiscal Intermediary (FI) to handle payroll and taxes. Many programs also provide a Support Broker to help you build your budget and find staff.7
2. Can I fire my own family member?
Yes. You are the employer. If a family member is not providing the care you need, you have the authority (and responsibility) to dismiss them, just like any other employee.2
3. Is self-direction available in every state?
Most states offer some form of self-direction, but programs vary wildly. Some restrict it to intellectual disabilities (IDD), while others (like California's SDP or New York's CDPAP) open it to broad populations. Check your state's 1915(c) waiver options.8
4. Can I use self-direction for just part of my care?
Yes. Many people use a "hybrid" model, using an agency for overnight nursing while self-directing their daytime community support access.3
5. How do I get started?
Contact your local Medicaid office or regional center. Ask specifically about "participant-directed options" or "employer authority" waivers.
Conclusion
Self-direction is not just a healthcare program; it is a civil rights advancement. It recognizes that disability does not erase the right to autonomy.
By shifting power from institutions to individuals, we don't just get better health outcomes—we build a society where people are defined by their choices, not their diagnoses.
Footnotes
-
National Inventory of Self-Directed LTSS. Documents the 1.52 million participant count. Reliability: Industry Standard Research. ↩ ↩2 ↩3
-
Medicaid.gov Self-Directed Services. Defines employer and budget authority. Reliability: Federal Agency. ↩ ↩2 ↩3 ↩4
-
MACPAC 2025 Report. Provides data on cost-effectiveness and unmet needs. Reliability: Federal Advisory Commission. ↩ ↩2 ↩3 ↩4 ↩5 ↩6
-
PHI National Direct Care Worker Report (2024). Contextualizes the workforce shortage. Reliability: Workforce Advocacy Data. ↩ ↩2
-
Sarah Taub Memorial Webinar. Highlights state-by-state variations. Reliability: Research Institute. ↩
-
NCI 2023-24 Report. Provides self-reported outcome data on inclusion. Reliability: National Data Aggregator. ↩
-
MyCIL.org Guide. Explains the roles of FIs and support brokers. Reliability: Center for Independent Living. ↩
-
AARP LTSS State Scorecard (2023). Confirms enrollment increases across 44 states. Reliability: Consumer Advocacy. ↩